Dr. Karen Horton has either authored or reviewed and approved this content.
Page Updated:
Please note: Our office is no longer a Participating Provider for insurance. We can provide a financial quote for what anticipated surgical fees will be after your consultation.
The Transverse Upper Gracilis (TUG) Flap is taken from the upper INNER THIGH region and uses skin, fat and a small piece of non-essential muscle from the inner thigh for breast reconstruction. A crescent-shaped flap of skin and fat is used to create a new breast mound using Microsurgery and the body’s own tissue, known as “autogenous tissue reconstruction”. The TUG flap has the same distribution as cosmetic thigh lift, and closure of the donor site creates a slender and attractive inner thigh donor site.
The TUG flap provides a permanent, warm, soft and shapely breast reconstruction, with a cosmetic result equivalent or sometimes even superior to the DIEP or the SIEA flap. The inner thigh flap also enables immediate nipple and areola reconstruction, which is a unique advantage of this reconstructive option.
During surgery, the crescentic designed flap is folded and shaped to provide increased projection to the reconstruction. The skin of the inner thigh flap is usually removed so that it lies beneath the natural breast skin in immediate breast reconstructions, to allow only the natural breast skin to be seen and just the soft fat of the flap to be felt. This is known as a “buried flap” beneath a skin-sparing or nipple-sparing mastectomy.
In the design of the TUG flap, tissue from the inner thigh is removed with some underlying skin, fat and a small amount of nonessential gracilis muscle. Unlike other major muscles of the body, the gracilis muscle is a thin, minor, expendable muscle that is not missed even if it is taken in its entirety (as is done for many other reconstructive procedures using Microsurgery). There is no “functional deficit” to removing a small piece of this muscle and there is no consequence to the inner thigh cosmetically. The purpose of including a small segment of the gracilis muscle with the flap is to ensure the most robust blood supply to the flap and promote Microsurgical success.
The inner thigh tissue is sculpted (“coned”) to create a shapely breast reconstruction with excellent projection and a natural breast shape. Like the DIEP and SIEA flaps, it is transferred “free in the air” and its blood vessels are reconnected under the microscope to blood vessels in the chest to reestablish the circulation to the flap.
The size of the TUG flap is sometimes slightly smaller than tissue that can be taken from the lower abdominal region. For this reason, the inner thigh flap can create a natural breast size and shape that often matches the volume of a woman’s natural breast, particularly if she does not have excessively large or pendulous breasts. Should a woman desire to have a larger breast reconstruction than the volume of tissue is available from the inner thigh region, additional options are available to further contour or augment the TUG flap in the future. Please read on to learn about options to individualize the cosmetic result of a TUG flap reconstruction.
Like all Microsurgical breast reconstructions, the TUG flap requires a team of specially trained and skilled Plastic Surgeon with Microsurgical expertise in breast reconstruction, up to a week’s hospital stay, and a slightly longer recovery than implant reconstruction. However, results of a TUG flap breast reconstruction are permanent, and no further surgeries are required after healing is complete.
Dr. Horton! I wanted to again say ‘thank you’ to you, Dr. Buntic and the staff at CPMC. You’ve helped me take the steps towards reclaiming my life after cancer and I’ll be eternally grateful. Thanks for your compassion, skill and for not giving up on me. - All the best, KT
„When the TUG flap is shaped during surgery, a natural projection to the breast reconstruction is created that simulates a nipple. Additional dissolving sutures are added to this projection to enhance the projection and create an immediate nipple reconstruction at the same time as the reconstruction.
Because the skin of the inner thigh region is naturally darker than the breast skin, an immediate areola reconstruction is also created if the nipple and areola requires removal during the mastectomy. Further tattooing of this area is often not necessary, although it is offered if additional pigmentation is desired, as an office procedure.
Like DIEP and SIEA flaps, if a nipple-sparing mastectomy is done at the same time as the reconstruction, the skin from the inner thigh flap is completely removed and the TUG flap is “buried” beneath the breast skin. The flap acts as a tissue “implant” and replaces the breast tissue with soft, warm, living tissue that feels just like a natural breast!
The DIEP or SIEA flap is often a primary choice for Microsurgical breast reconstruction due to the superiority of the tummy tissue over that of other donor sites such as the back or the buttocks, and the presence of excess tummy fat in many women.
However, if abdominal tissue is unavailable (previous abdominal flap or tummy tuck, significant past abdominal liposuction or an extremely thin tummy area), a free flap from the inner thigh area (the TUG flap) is an excellent choice for reconstruction of the breasts. Some women have little abdominal fat but significantly more inner thigh fat. In these women, the TUG flap is in fact their best reconstructive option based on their body shape and fat distribution.
If no donor site tissue is realistically available from either the tummy or inner thigh area, an implant may be recommended. Please see our Breast Implant Reconstruction section for information on our state-of-the-art single stage breast implant reconstruction procedure.
Please see our Preparing for Surgery section to learn about what actually happens in the operating room on the day of surgery.
For immediate reconstructions, the mastectomy and elevation of the TUG flap occur at the same time, which decreases total time under anesthesia. Two separate surgical teams (the Breast Surgeon and two Microsurgeons working as a team) operate in tandem. Measurements of the breast tissue are taken as a reference point for your reconstruction.
The TUG flap is supplied by an artery and 1-2 veins, known as the “microvascular pedicle” which brings blood flow to and from the inner thigh flap tissue. Once the inner thigh flap has been “elevated” on its specific blood vessels, the blood vessels are divided and it is ready to be transplanted to the chest area.
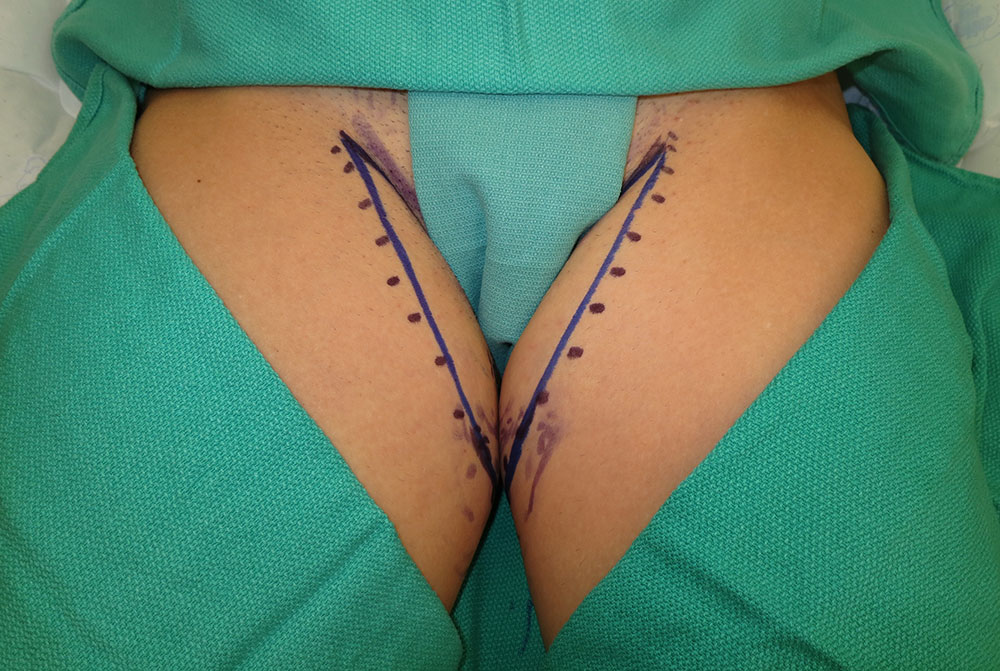
Intraoperative markings of the TUG flap. The majority of tissue taken is from the back of the inner thigh.
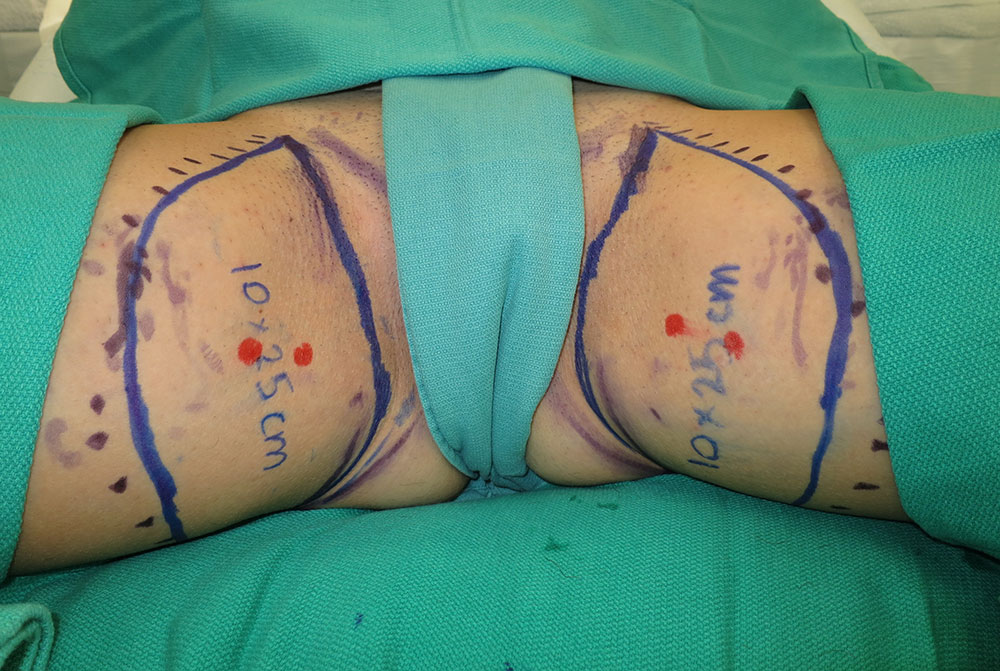
The inner thigh TUG flap takes fat and skin from the upper inner thighs to reconstruct soft and natural breasts. The dots indicate additional fat that will be included with the flap elevation.
The inner thigh area does not “miss” the blood vessels that have been used for the flap; many other blood vessels in the donor site area take over the circulation to the remaining abdomen or thigh. Nerves are not taken with the flap. Sensation will slowly recover in the donor site area over many months after surgery, and nerves commonly gradually grow into the flap to provide some sensation.
The inner thigh region also does not “miss” the gracilis muscle, which is a minor adductor muscle. The large and strong adductor longus and adductor magnus muscles take over the function of the small, thin gracilis muscle, and its removal does not leave any contour defect or functional deficit.
The blood vessels of the flap are then reconnected (“reanastomosed”) to recipient blood vessels found beside the sternum in the chest area. The recipient vessels most commonly used are the INTERNAL MAMMARY ARTERY AND VEIN. In order to access these blood vessels, a small segment of rib cartilage is removed, as the vessels lie protected underneath. Removal of this cartilage does not create any pain or deformity, the body does not “miss” it and the chest is not affected in any way. The internal mammary blood vessels are the recipient vessels of choice for breast reconstruction; they provide excellent circulation to the flap in the chest and are available for Microsurgery even after radiation.
The inner thigh flap artery and vein are reanastomosed (surgically repaired) to their recipient vessels under the operating microscope. The flap is literally “transplanted” from one part of the body to another using Microsurgery to disconnect and then reconnect the blood vessels in their new location. However, unlike an organ transplant from one person to another, there is no chance of rejection of the TUG flap because the donor and recipient is the same person! Microsurgery truly enables rearrangement of a woman’s own body to provide her with the most natural form of breast reconstruction.

Front: TUG flap inner thigh scars are barely visible from the front, even in bikini bottoms.
Back: From behind, the TUG flap scar is hidden in the fold of the buttocks. Most women have a “thigh gap” after TUG flap surgery!
For the inner thigh (TUG) flap, the inner thigh incision is closed to create a lifted and thinner inner thigh, like a thigh lift. Drains are inserted into the flap site and the donor area and typically remain in place for 1-2 weeks. Each breast reconstruction will also have a drain that is in place for up to a week.
I can only say Dr. Horton completely changed my life. I had numerous unsuccessful surgeries before finally meeting Dr. Horton. I was a 2 time cancer survivor and the radiation from my initial diagnosis breast caused substantial damage and made reconstruction very difficult. I had unsuccessful breast reconstruction after my bilateral mastectomy at UCSF. She patiently talked to me about options and gave me the bad news that my body would need to heal for a year from ongoing inflection I had from my surgeries with my prior doctor. She told me what I needed to hear, not what I wanted to hear. I had numerous stages to my reconstruction. Dr. Horton and I talked about how there would be a number of steps needed, for my initial surgery with her I underwent a free flap surgery. She was with me very step of the way. She gave me her cell phone number and I called me immediately if I texted or left her a message. She was always there to assure me when I was concerned. I am sad to see the negative comments. I am confident that Dr. Horton never told anyone that all they would need is one surgery. No doctor can guarantee results nor outcomes. Every person is different and their bodies respond differently. I had to have additional surgeries due to healing issues with my breast bone. (again my body issue, not Dr. Horton) She gave me a “makeover” and I am so happy with the outcome. I look and feel better than I have in 20 years! I sent one of my best friends to Dr. Horton when she was diagnosed with Breast Cancer. She loved Dr. Horton and had the same amazing experience that I did. The preponderance of comments are positive and reflect who Dr. Horton really is. I have, and will continue, to recommend her. She is truly the best.
„Microsurgery is only performed at specialized Microsurgical centers of excellence such as the Davies Campus of California Pacific Medical Center (CPMC). Microsurgery was “born” at this center in North America over 40 years ago, and complex reconstructive cases are performed here every single day, including numerous Microsurgical breast reconstructions. We choose to bring our patients to this hospital because of the skilled, expert Microsurgery Nurses, the experienced operating room staff, and the warm and wonderful hospital staff in general.
Please print out and read the comprehensive Preparing for Breast Reconstruction Surgery handout. Prepared by Nurses and Doctors at Davies, this pamphlet describes in detail how to prepare for breast reconstruction surgery, educates you what to expect in the hospital, your recovery and explains postoperative recommendations specific to your type of breast reconstruction.
You will spend approximately seven nights in the hospital after a Microsurgical free flap breast reconstruction. Your breast drains and implantable venous Doppler probe monitors will be removed before you leave the hospital. We will see you back in the office a few days after you go home to remove your donor site drains, and approximately 3-6 weeks after that to check on your wound healing.
It is recommended that you do not exercise, lift more than 5 pounds, or do any activities that raise your heart rate and blood pressure for approximately 4-6 weeks after surgery. At 6 weeks after flap surgery you can return to your usual activities without restriction. However, “listen to your body” is the rule, and if it feels like you are straining even after six weeks, be sure to avoid activities or movements that are still creating discomfort. Remember that is takes many months for your body to fully recover after any form of surgery. Breast reconstruction is no exception. Your body will let you know when it is ready to gradually resume strenuous activities.
Dr. Karen Horton was recently interviewed by Terri Coutee, founder of the DIEPcFoundation, about TUG flap microsurgical breast reconstruction. Watch the video below for details.
TUG Flap Breast Reconstruction
When you are considering any type of surgery, you should be fully educated about potential risks and complications. Please see our Preparing for Surgery section for information relating to surgical procedures in general.
When specifically considering Microsurgery, there are some additional details to recognize:
After most types of Microsurgery, very quiet physical activity in your hospital bed for up to five days is recommended to allow the blood vessels to mend without complications. During this time, you may move around in bed and flex your calves to keep the blood flowing in your legs. A bladder (“Foley”) catheter is in place, and you will not likely need to have a bowel movement during this time due to slight normal constipation from anesthesia and pain medications. To prevent against blood clotting, you may be placed on an intravenous blood thinner temporarily after surgery, and can expect to take a daily aspirin orally for a month after surgery. You will also be instructed on deep breathing and coughing to keep your lungs fully expanded and healthy while in the hospital.
In the vast majority of cases, Microsurgery is a success! There is a 1-2% risk of “Failure” Of The Microvascular Anastomosis in our experience, which is lower than the published literature. Recall that a tiny (2-3 mm diameter) artery and vein are reconnected together under the microscope. There is a remote chance of a “thrombosis” (clot or obstruction) of the vessels providing circulation to the breast flap early after surgery. If the flap circulation becomes blocked for some reason, the flap could fail and require removal.
A problem with the free flap circulation statistically occurs most often in the first 24 hours after surgery. It is for this reason that intense monitoring of the flap circulation takes place in the hospital (TICU or step-down unit) for the first 5 days after surgery, and up to a full week’s stay is recommended – to ensure success of the operation! When you are discharged from the hospital, the risk of thrombosis or flap complications is generally over.
During your hospital stay, specially trained Microsurgery Nurses will monitor your flap circulation in a number of ways:
(1) “Clinical Monitoring” consists of assessing the flap at regular intervals by inspection (looking) and palpation (feeling) the tissue to ensure it is warm, pink, with a normal amount of swelling and capillary refill. (2) If there is exposed flap skin, a Pencil Doppler Probe (similar to probes used to assess fetal heart beats in pregnant women) will assess the flap circulation, and (3) an Implantable Venous Doppler Probe will be temporarily implanted at the time of surgery to monitor the flap circulation by way of a real-time, “Doppler radar” audible signal of blood flow.
It takes approximately five days after Microsurgical anastomosis for the internal lining of the blood vessels to mend. Once you are ready to leave the hospital, all monitoring is discontinued. The risk of a flap complication is generally over after five to seven days postoperatively. You do not need to continue any special monitoring at home.
Should there be a concern about the flap circulation while in the hospital, you will immediately return to the operating room for your Microsurgeons to assess your flap and to repair or redo the anastomosis if necessary. The incidence of a Microsurgical “take back” is very low, but should a flap circulation problem occur, your surgeons will usually be able to fix the problem without any consequences. Should the flap circulation problem persist, the flap would require removal and another reconstruction type could be discussed in the future. Flap failure is extremely rare and does not pose any risk to your life or your health should it occur.
After a flap breast reconstruction, mild differences may exist between the breasts. At the time of nipple and areolar reconstruction (if needed) or approximately 6 months after a flap, minor revisions can be performed to optimize the appearance of the flap and the other breast. Flap revision can include contouring of the flap by removing fat using liposuction or by surgical revision, performing a “lift” of the flap or scar revisions to make the breasts as symmetric and attractive as possible.
Sometimes after a free flap breast reconstruction, a breast implant is placed beneath the flap for enhanced projection and better symmetry with the other breast. A waiting period of at least 6 months is recommended after Microsurgery before an “augmentation” of the flap is done. Either a postoperatively adjustable saline implant or a silicone gel implant can be placed, depending on the aesthetic goals and the degree of flap augmentation planned.
Augmentation of a flap is considered a revision of the breast reconstruction and is usually covered by insurance. Whereas an implant-based breast reconstruction has unique risks and complications, augmentation of a flap is much more similar to a breast augmentation. The flap tissue provides additional padding over the implant, preventing it from being visible and palpable like an implant reconstruction, and the risk of complications is closer to a breast augmentation than an implant reconstruction.
Occasionally, free fat grafting (also known as “lipofilling”) can help to fill in contour defects around a breast reconstruction. Fat can be taken (“harvested”) from one area of the body using a liposuction cannula and transferred to fill in an area that is not fully corrected by traditional reconstructive methods (for instance, above the breast reconstruction below the collarbone or in a hollow resulting from axillary lymph node dissection). Fat grafting is only used as an adjunct to special reconstructive situations and is generally not recommended in routine cosmetic procedures.
When fat is transferred by lipofilling, some of the fat will survive and some cells do not. Calcifications can form in the area of fat grafts that do not “take” (survive); this can show up as abnormalities on a mammogram. For this reason, free fat grafting is only recommended in small areas where there is not normal breast tissue, such as in Poland Syndrome or after mastectomy and reconstruction. Correction by lipofilling may be complete after one session of fat grafting, or a 2-3 procedures staged 3-6 months apart may be needed; surgery is done in the operating room as an outpatient procedure.
After any surgical procedure, areas of raised skin or protuberant soft scars nicknamed “dog ears” (raised points of skin and/or fat) can occur at the very end of the incisions. This can happen both after a mastectomy and at the donor site scars. Very often, raised areas of swelling slowly resolve over six months to a year after surgery. Occasionally, if dog ears persist, a scar revision can be done 6-12 months after the flap to trim any excess skin and fat, creating a flatter end to the donor site incision. Scar revision surgery is covered by insurance and is done together with any other procedures planned at the final surgery (nipple and areola reconstruction, flap revision, donor site contouring, fat grafting).
Our goal is not only to create the most beautiful breast reconstruction possible but also the most aesthetic donor site. Our flap reconstruction patients are often excited and proud to show off their new bodies in a bikini! Following a flap reconstruction, most women do not need any additional surgery.
However, many breast cancer survivors are interested in additional contouring of their donor sites after their flap to flatten their tummies or further thin out their thighs. The method used most often for donor site contouring after a TUG flap harvest is Liposuction. Liposuction effectively removes stubborn deposits of excess fat that persist even after surplus fat is used for breast reconstruction. Unfortunately, liposuction is not covered by insurance and is considered cosmetic.
If a cosmetic procedure such as donor site liposuction (or another cosmetic procedure) is being contemplated, then planning it as a compliment for the reconstructive procedure (flap revision, scar revisions, etc.) in the same operation is a wise option.
Combining reconstructive and cosmetic procedures at the final surgery lessens total time under anesthesia, limits the recovery period, and enables the very best aesthetic results of both the breasts and the tummy or inner thigh! In benevolence to our patients, we usually offer a discount on cosmetic procedure fees when they are added to their final breast reconstruction procedure. Please contact our Patient Coordinator Mary Pasache in our office to discuss applicable cosmetic fees.
Patients often travel for breast reconstruction and Microsurgery at our practice. Women seeking free flap and perforator breast reconstruction come from other regions of the United States and sometimes other parts of the world.
Our patients recognize that specialized breast reconstruction is not offered in every city or state; they travel to San Francisco to receive superior attention and care. Please see our Online Reviews section to hear about our breast reconstruction patients’ experiences in their own words.
Please contact our Patient Coordinator Mary Pasache to learn more about visiting us for a TUG flap breast reconstruction consultation.
Dr. Karen Horton has either authored or reviewed and approved this content.
Give us a call or fill out form below to schedule online.
Dr. Karen M. Horton
2100 Webster St UNIT 520
San Francisco, CA 94115
Phone: 415.923.3067
We are located in the Pacific Heights District in the Pacific Professional Building.
Monday-Friday: 9am - 5pm
Saturday-Sunday: Closed
Monday:
9 AM to 5 PM
Tuesday:
9 AM to 5 PM
Wednesday:
9 AM to 5 PM
Thursday:
9 AM to 5 PM
Friday:
9 AM to 5 PM
Saturday:
Closed
Sunday:
Closed
Dr. Karen M. Horton
2100 Webster St UNIT 520
San Francisco, CA 94115
Phone: 415.923.3067
We are located in the
Pacific Heights District
in the Pacific Professional Building.
 SHOP SKIN CARE
SHOP SKIN CARE*Please note: Our office is no longer a Participating Provider for insurance. We can provide a financial quote for what anticipated surgical fees will be after your consultation.