Breast Implant Illness (BII) treatment: “En Bloc” capsulectomy not necessary for explantation
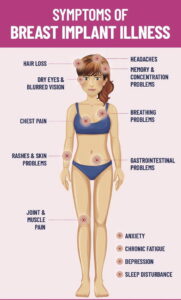
What is “breast implant illness” (BII)? BII is a controversial current term born from social media, and is a poorly understood phenomenon of wide-ranging and non–organ-specific range of symptoms that can develop after breast implant reconstruction or cosmetic breast augmentation; however, BII is not clearly defined as an official medical diagnosis. Symptoms include fatigue, brain fog, joint pain, anxiety, hair loss, depression, rash, autoimmune diseases, inflammation and/or weight problems. Breast implant illness is being studied in the scientific literature by several of my colleagues. While I rarely see patients complaining of these symptoms, I feel it’s important to share what we know about BII treatment.
When I see patients who are interested in having their breast implants removed, we usually discuss explantation in the office under local anesthesia with an oral anti-anxiety mediation and dilute laughing gas to make the entire procedure more pleasant. Explantation surgery should be a straightforward procedure, offered to women as a simple outpatient surgery when they no longer want their breast implants. It takes around an hour, no drains are required, patients can shower in 2 days and return to exercise in 10-14 days. See before and after images of explantation surgery here.
Rarely is a total “en bloc” capsulectomy required – which refers to an extensive and lengthy (2 hours per side) removal of the entire breast implant with its surrounding scar tissue capsule intact – and that requires general anesthesia, a LONG incision under the breast, drains in place for weeks, and puts the underlying ribs and lung at risk for injury when the breast implants are under the muscle. For patients with significant capsular contracture who wish to have their implants removed and/or replaced, sometimes a breast revision involving a localized (but incomplete) capsulectomy is done to remove thick scar tissue that is creating deformity.
Unfortunately, there are some physicians out there that are recommending en bloc capsulectomies for every patient who wishes to have their implants out, consequently feeding into fear and misinformation about who needs to have their entire capsule removed. En bloc removal of capsular tissue is a “morbid” procedure with significant downtime and recovery, bleeding, pain and scars. En bloc capsulectomy is only recommended by the FDA and our professional societies to treat anaplastic large cell lymphoma (ALCL), a rare subtype of lymphoma that has found to be related to textured breast implants. In cases where ALCL is not suspected, removal of the entire capsule around the breast implant is not necessary.
Several of my female Plastic Surgery colleagues are studying women with self-described breast implant illness. A study published in Aesthetic Surgery Journal in December 2021 investigated whether simple removal of the breast implant with limited capsulectomy had different outcomes in alleviation of BII symptoms when compared to partial capsule removal (limited capsulectomy) and total en bloc capsulectomy.
What the study found was prospective (looking forward in time), blinded (the evaluators did not know which group the patients were in) and had three groups of patients (cohorts):
- Women with self-described BII;
- Women with implants undergoing exchange or removal without symptoms they attribute to their implants; and
- Women undergoing mastopexy who have no history of any implanted medical device.
The study included self-reported symptom surveys, including anxiety, fatigue, cognitive function, and sleep disorders. Reports were gathered at baseline, 3-6 weeks, 6 months and 1-year after surgery, with 80-98% follow up at 6 months. Scar tissue (capsule) from around the breast implants were collected together with peripheral blood samples the day of surgery. The type of capsulectomy performed was recorded as en bloc, complete, or partial, and capsules and implants were photographed. Capsules were also sent for heavy metal testing (22 metals), PCR, and pathology, including peripheral blood testing for CRP, CBC, thyroid, Vitamin D, cytokines, and IgG and IgE antibodies to Staph toxins. The results of this testing will be reported in Part 2, the second paper in this series (which I will share once it is published).
The results of Part 1 of this study looked at symptom relief after capsulectomy. At 6 months, with 98% follow up, 94% of the BII subjects had similar symptom improvement, and it was independent of the type of capsulectomy performed:
“The type of capsulectomy; intact total, total, or partial all showed similar symptom improvement with no statistical difference in the reduction of symptoms based on the type of capsulectomy.”
Compared to the 2 control cohorts, the BII cohort had significantly higher reported presence of all symptoms, and in the symptom surveys, significantly higher anxiety. Both symptoms and anxiety improved in the BII cohort, but never to the levels of the control groups.
Impact of this BII Study: Prior research recommended en bloc capsulectomies for ALCL treatment only, and when concerns related to textured breast implants and ALCL symptoms existed. Despite the lack of scientific support, practitioners began recommending exclusively en bloc capsulectomies for BII patients, a practice noted as a social media phenomenon. This study now confirms that en bloc capsulectomies for BII patients provide symptom relief no better than total or partial capsulectomies.
Our professional societies are recommending that Plastic Surgeons “follow the science”, which in this case is directing us to avoiding unnecessary surgery such as en bloc capsulectomy for BII.
 Ethical Considerations recommended by The Aesthetic Society: Board Certified Plastic Surgeons are expected:
Ethical Considerations recommended by The Aesthetic Society: Board Certified Plastic Surgeons are expected:
- To keep abreast of scientific knowledge (AMA Principles of Medical Ethics);
- To “only practice based upon a scientific basis” (The Aesthetic Society Code of Ethics, Section 1.02(b) and ASPS Code of Ethics, Preamble); and
- To advance “the art and science of plastic and reconstructive surgery.” (ASPS Code of Ethics, Section 1: General Principles III).
This recent study demonstrates that promoting en bloc capsulectomies as the exclusive treatment for symptom relief for BII patients is not evidence-based, and may well subject surgeons to needless liability when their motives are challenged by attorneys representing BII patients who are dissatisfied with the impact of their now suspect en bloc capsulectomies.
As one of the study authors, Dr. Patricia McGuire expressed to me personally when I asked for her comments on the study: “I think it is important to acknowledge that these patients have real symptoms, they are not hypochondriacs. We showed their symptoms at least partially improved after implant removal despite the type of capsulectomy performed. This is good news for patients because, although there is no guarantee that their symptoms will improve with explant, they don’t need an “en bloc” capsulectomy which requires longer surgical time, anesthesia and carries a higher risk. The next question is why do they get better. That’s what we look at in the next parts of our study where we evaluated capsules for heavy metals and bacterial and fungal DNA. We wanted to add scientific evidence into the BII discussion.”
So to summarize, explantation surgery does not always require extensive surgery and can help women who are worried that their breast implants are causing vague symptoms. The Plastic Surgery community is currently researching “breast implant illness” and evidence-based medicine will provide additional knowledge. I don’t feed into fearmongering associated with BII; instead, I take great care of patients one at a time, and do my best to find the very best solution for each woman.