Mammograms with breast implants – Q & A with Dr. Horton
Dr. Horton recently had her annual mammogram at the CPMC Breast Health Center and was inspired to share some important information about breast health and breast cancer screening with breast implants, as she is a breast augmentation patient herself.
Here are some common questions and important answers regarding getting mammograms after a breast augmentation:
Does having a mammogram hurt?
Having a mammogram feels tight like firm pressure on your breast but does not usually hurt – even if you have breast implants. At your mammogram appointment, you change into a comfortable robe and are escorted to a private room with a standing X-ray machine (see above) that has arms that rotate in different angles. The mammogram technician is usually female (I have never seen a male technician in my half-dozen-or-so mammograms to date, although I’m sure men would do a fabulous job too!).
During a mammogram, your breast is placed on a flat support plate and compressed with a parallel plate called a paddle. An X-ray machine produces a small burst of energy that passes through the breast to a detector located on the opposite side. The detector is either a photographic film plate which captures the x-ray image on hard film, or a solid-state detector, which transmits electronic signals to a computer to form a digital image.
Your breast will be positioned into position between the plastic plate and paddle, which are then tightened together to flatten and hold your breast tissue still for imaging. During each view (3 images per breast), you are instructed to hold your breath for around 5 seconds as energy is transferred between the plates to visualize your breast tissue. If you have particularly tender breasts around ovulation or menstruation, then you might want to try to schedule your appointment at a time in your cycle when your breasts are not usually sore or take Tylenol or Ibuprofen an hour before your appointment.
What is a mammogram exactly?
A mammogram is an X-ray examination of your breast taken from different angles. Mammograms are recommended to start at age 40 and occur yearly to look for signs of cancer or abnormalities in the breast, such as a tumor (mass or lump), calcifications, areas of abnormal density or cysts. On the image, breast tissue looks white on the imaging; fat looks black. Regular mammograms can find signs of breast cancer early such as calcifications, sometimes up to three years before a lump can be felt clinically.
Mammography has been around for over 30 years, and in the past 15 years technical advancements have greatly improved both the technique and results. Dedicated imaging equipment used only for breast X-rays produces studies that are high in quality, but low in radiation dose. Unlike other types of X-rays where your thyroid gland and genitalia are protected with a lead apron, radiation risks with mammography are considered to be negligible.
Most centers perform digital mammography now (rather than regular X-rays on hard film). Digital mammography provides electronic images of the breasts that can be enhanced by computer technology, stored on computers, and even transmitted electronically in situations where remote access to the mammogram is required. Interestingly, AI (artificial intelligence) is starting to be used as an adjunct to human Radiologists to help detect abnormalities that could be missed by the human eye.
Can mammograms cause breast implant rupture?
No! Biomechanical studies have shown that it takes fifty times the force of a mammogram to cause a breast implant to rupture. I previously believed that a high-velocity car crash would be powerful enough to rupture an implant. However, I have had a few patients (thankfully) survive severe motor vehicle collisions that caused significant bruising to their ribs and chest wall. We were concerned about implant rupture, so we ordered an MRI of the breasts – MRI imaging is the most effective way to detect breast implant rupture. Despite the MRI reporting that the implants were intact, I took these patients back to the O.R. to inspect the implants, which were indeed fine!
What I have seen predispose to breast implant rupture in the long term (over 10+ years) is placement of implants under the muscle – the muscle contracts against the implant and can create a crease or bend in the implant shell every time the pectoralis major muscle contracts (literally hundreds of times each day). This is called an “animation deformity” – see a video of my patient demonstrating this here.
Chronic folding of the implant surface can eventually cause weakness in that area and result in a “fold flaw” in the implant shell, with subsequent and implant “rupture”. I dislike the term rupture because if a modern silicone breast implant shell were to break, the implant does not explode! Any silicone material tends to stay within the pocket of the breast and remain “intracapsular” – perhaps the term “implant shell fracture” would be more accurate. The risk of fold flaw with muscle contraction is one reason I prefer implant placement on top of the muscle (subglandular or prepectoral placement).
Is it harder to detect breast cancer with mammography with a breast implant in place?
No – in fact, several studies have revealed that if a woman were to develop a breast lump, it is actually easier to feel the lump when a breast implant is present. This is not to say that having breast implants is protective, but the implant makes it easier to palpate (feel) a new growth or mass if it were to develop.
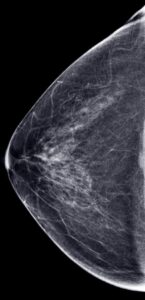
Below are my actual mammogram images from a month before I had my breast augmentation in 2019. My breast tissue is dense (very white) with little fat, so the image does not have much black space.
For breast cancer screening, does it matter whether a breast implant is over the muscle or under the muscle?
It does not matter whether an implant is under the muscle (submuscular, subpectoral) or on top of the muscle (subglandular) with respect to mammograms’ effectiveness. When you arrive for your mammogram, you will complete a questionnaire asking about past breast surgeries, breast cancer treatment, and whether you have breast implants.

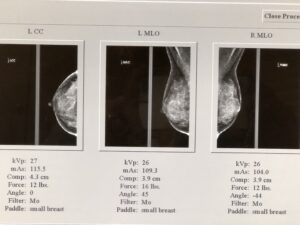
My mammograms with breast implants – the implant is seen as the large white half-dome, and the breast tissue is visualized on top and around the implant
How can I be sure the mammogram is visualizing all my breast tissue if I have breast implants?
In addition to the standard views, additional implant displacement (ID) views – I call these the “horizon views” (see below) are taken when you have breast implants. The breast tissue is displaced forward off the implant, and is visualized lying overtop of the implant, as seen in my own mammograms, above. The implant is pushed back against the chest wall and the breast is pulled forward over it and then compressed. This allows better imaging of the front part of each breast so the doctor can get a better look at the breast tissue.
At what age should screening mammograms start and how often should you have a mammogram?
The American College of Radiology (ACR) and the Society of Breast Imaging (SBI) recommend that women get yearly mammograms starting at age 40. In May 2023, the U.S. Preventive Services Task Force (USPSTF) updated its recommendations to begin breast cancer screening at age 40 since data shows that 1 out of 6 new breast cancers develop in people who are in the age range of 40 to 50. Cancers detected during screenings are usually early stage, and the earlier we catch a cancer, the better the prognosis and survival rate for the patient.
If you have a family history of breast cancer, particularly in a first-degree relative (mother or sister) or if you are a carrier of the BRCA gene, then your annual screening should begin around 10 years before that family member was diagnosed with breast cancer. Mammograms are usually ordered by your Family Doctor or OB-GYN, but we can always refer our patients to a local breast health center for imaging if needed.

Our office is located in the building immediately next to the Pacific Campus of CPMC, where we refer for mammograms
How long after having breast surgery should I wait before my next mammogram?
We usually recommend waiting at least 6 months after surgery of the breast before scheduling your next mammogram. This time period will allow surgical swelling and postoperative discomfort to resolve, and facilitate the most accurate imaging of the breast.
I hope you find this information helpful. If you have questions about breast cancer screening or breast health, please contact your Primary Care Physician or Obstetrician-Gynecologist for guidance.
Want to receive alerts about future blog posts when they are published? Complete this form and you’ll be the first to know!
REFERENCES:
https://www.cdc.gov/cancer/breast/basic_info/mammograms.htm
https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/mammogram-procedure
https://www.nibib.nih.gov/science-education/science-topics/mammography
https://www.nationalbreastcancer.org/mammogram/
https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/mammograms/mammograms-for-women-with-breast-implants.html
https://www.sutterhealth.org/ask-an-expert/answers/breast-implants-cancer-detection
https://pubmed.ncbi.nlm.nih.gov/29595718/
https://pubmed.ncbi.nlm.nih.gov/18090816/
https://pubmed.ncbi.nlm.nih.gov/25057749/